Hospital delirium, in pre-pandemic times, was the most common complication
among hospitalized patients ages 65 with upwards of 30% for those on a regular
medical ward and up to 50% for those having a surgical procedure. That’s staggering.
Patients who suffer from hospital delirium have worse outcomes, longer hospitalizations
and more complicated recoveries.
Studies have shown that families at bedside can play an essential role in both
identifying delirium at an early stage but also preventing it – by grounding the patient in
the familiar things of their regular life; monitoring pain; protecting sleep and
safeguarding hydration and nutrition.
But the coronavirus pandemic has separated families and friends from a
hospitalized loved one. And reports are noting that isolated patients are at a far greater
risk for delirium. Hospitals have zero or highly restricted visitation policies in place for
the safety of all staff and patients but isolation, loneliness, immobility and undertreated
pain are severe stressors on healing and also significant contributing factors towards
developing hospital-based delirium. How can families help to protect their loved one if
caregiving is mostly done remotely during these difficult times?
First, it’s important to know the signs of hospital delirium which can include a
sudden change in mental status; difficulty focusing; impaired memory; restlessness;
insomnia; daytime sleepiness and either being too quiet or too agitated. This is where
the family’s expert knowledge of who the patient is in normal life can play a crucial role
in alerting staff that something is very wrong.
Second, it’s important to be familiar with some of the causes of hospital delirium:
dehydration; medication side effects; interrupted sleep; being bed bound; the stress of
illness or injury amidst the disorienting hospital setting. When family is at bedside they
can help alleviate some of these stressors but with remote caregiving families need
practical workarounds to monitor risk factors and try to short-circuit concerns before
they become real problems.
How family can help:
- Keep in regular touch with your loved one over the phone but also via Facetime.
Eyes on your loved one can alert you to changes in mental status. You know
best if they don’t seem like themselves. Alert the staff if you think something is
wrong. Facetime daily – and if your loved one is too fragile to manage this – ask
your nurse for a regular check-in when she or he is rounding. - Make conversations about familiar people and events a regular part of any
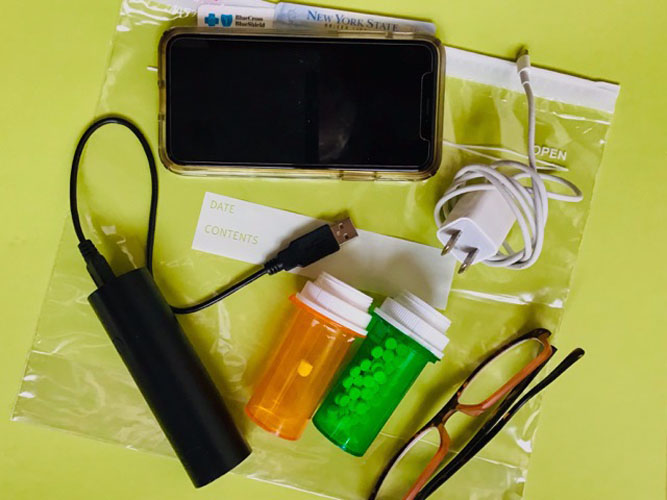
conversation to orient them to their normal life. - Make sure your loved one is using their sensory aids: hearing aids, glasses and
dentures if they need them. Not using them can create a cascade of
disorientation in the unfamiliar setting of the hospital. - Work with the hospital staff to normalize day and night for your loved one– open
the shades during the day, encourage wearing a sleep mask at night, ask that
any disruption to sleep be kept to a minimum. - Keep track of hydration and nutrition. Dehydration is a completely avoidable risk
factor for hospital delirium - Keep track of all medications. Ask for a medication review to see if certain meds,
like sleeping pills or tranquilizers, that are commonly dispensed in hospitals could
contribute to delirium. Are they necessary? Is pain medication adequate?
Undertreated pain is a major stressor that contributes to hospital delirium.
Adapted from The Patient’s Checklist: 10 Simple Checklists to Keep You Safe, Sane
and Organized. © 2020 Elizabeth Bailey